CARE FOR TODAY AND TOMORROW
Heart Attack
A myocardial infarction, commonly known as a heart attack, constitutes a critical medical situation in which the heart muscle starts to perish due to inadequate blood circulation. The typical cause is an obstruction in the coronary arteries, the vessels responsible for supplying blood to the heart. If medical intervention to reestablish blood flow is not promptly administered, a heart attack can lead to irreversible damage to the heart and prove to be fatal.
What Is A Heart Attack?
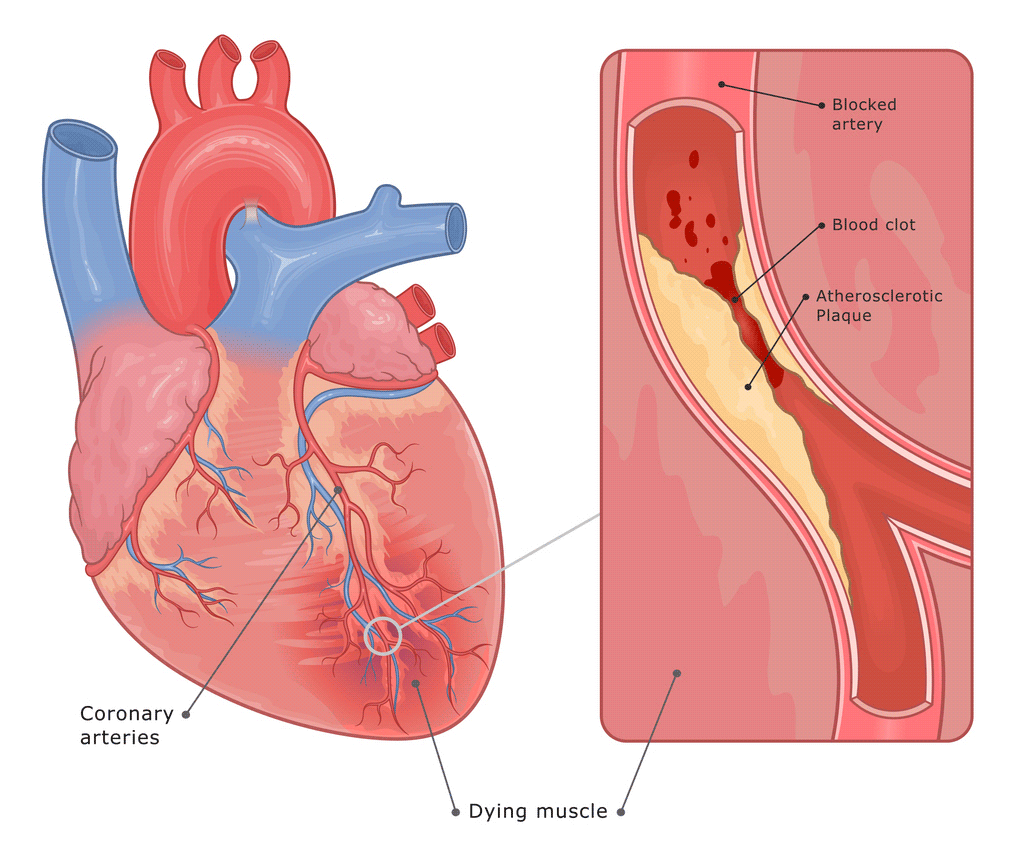 A heart attack, commonly referred to as a myocardial infarction, is a critically dangerous situation that occurs when there is insufficient blood supply to part of the heart muscle. Various reasons can trigger this reduction in blood flow, but it most commonly happens due to a blockage in the arteries that supply blood to the heart.
A heart attack, commonly referred to as a myocardial infarction, is a critically dangerous situation that occurs when there is insufficient blood supply to part of the heart muscle. Various reasons can trigger this reduction in blood flow, but it most commonly happens due to a blockage in the arteries that supply blood to the heart.
In the absence of adequate blood supply, the portion of the heart impacted will start to deteriorate and die. Quick action to restore blood circulation is essential. Without prompt intervention, a heart attack may lead to irreversible damage to the heart or even prove deadly.
Recognizing a heart attack as an urgent medical crisis is vital. If you or someone around you shows signs of having a heart attack, please call 911 immediately (or the appropriate emergency services number in your region). The timing in addressing a heart attack is crucial; slight delays can lead to permanent damage to the heart or fatal outcomes.
How common is a heart attack?
Every year, more than 800,000 people in the U.S. have a heart attack. Most heart attacks are due to coronary artery disease, which is the most common cause of death in the United States.
What Occurs During A Heart Attack?
During a heart attack, a section of the heart receives significantly reduced blood flow or none at all, leading to damage or death of that heart muscle segment. The lack of blood flow causes the affected area to lose its ability to pump effectively, impairing the overall pumping mechanism of the heart. This impairment can decrease or completely halt blood circulation to the body, posing a potentially fatal threat unless promptly addressed.
Is My Heart Permanently Damaged?
When a heart attack occurs, the heart muscle that has lost blood supply begins to suffer injury. The amount of damage to the heart muscle depends on the size of the area supplied by the blocked artery and the time between injury and treatment.
Will I Recover From My Heart Attack?
The good news is that recovery from a heart attack is likely. The heart muscle begins to heal soon after a heart attack and usually takes about eight weeks. Scar tissue may form in the damaged area, and while it does not contract or pump like healthy muscle tissue, the heart can still function. The extent of damage to the heart muscle can impact how well the heart pumps blood throughout the body, but the degree of loss of function depends on the size and location of the scar tissue.
Why Didn’t I Have Any Warning?
Not experiencing any warning signs before a heart attack can be alarming and confusing. Heart attacks can occur without prior warning for several reasons, and understanding these can help in recognizing the subtle risks and taking preventive steps. Here’s why you might not have had warning signs:
Asymptomatic Conditions
Some individuals have underlying heart conditions or risk factors that do not present noticeable symptoms. Conditions such as high blood pressure or high cholesterol can silently contribute to the narrowing of arteries over time without any outward signs, leading to an unexpected heart attack.
Silent Ischemia
Silent ischemia is when the heart muscle receives insufficient blood flow (ischemia) without producing the typical chest pain or discomfort (silent). People with silent ischemia may have heart attacks without prior warnings because they do not feel the usual symptoms due to differences in pain tolerance, diabetic neuropathy, or other reasons.
Atypical Symptoms
Some heart attacks present with atypical symptoms that may not be immediately recognized as heart-related. These can include shortness of breath, fatigue, nausea, dizziness, or discomfort in jaw, neck, or back areas. These symptoms might be mistaken for other, less critical conditions, delaying recognition of a heart attack.
Plaque Rupture
A heart attack can occur suddenly due to the rupture of a cholesterol plaque in a coronary artery. The rupture leads to the formation of a blood clot, which can quickly block an artery. This blockage might happen so rapidly that it doesn’t provide any noticeable warning signs before the onset of a heart attack.
Individual Differences
Everyone experiences heart problems differently due to variations in pain thresholds, health conditions, and lifestyle factors. Some people might not recognize or attribute mild symptoms to heart issues, especially if they have a higher pain tolerance or if the symptoms don’t fit the classic heart attack depiction.
The absence of warning signs before a heart attack underscores the importance of regular health screenings and being aware of the less typical symptoms of heart issues. Lifestyle modifications to reduce heart disease risk—such as maintaining a healthy diet, exercising regularly, avoiding smoking, and managing stress—can also play a key role. If you have risk factors for heart disease, discussing them with your healthcare provider can help in managing these risks more effectively and possibly prevent future heart events.
Recognizing the Symptoms of a Heart Attack
A heart attack is a life-threatening event that requires immediate attention and medical intervention. Understanding and recognizing the symptoms of a heart attack quickly can significantly improve survival rates. Here, we outline the common and less common symptoms to watch for:
Common Symptoms
Identifying these symptoms early can be key to receiving prompt treatment:
1. Chest Pain or Discomfort
The most recognizable symptom of a heart attack is intense discomfort in the chest, often described as feeling like an elephant is sitting on one’s chest. This pain or pressure can last more than a few minutes or go away and come back. It can feel like uncomfortable pressure, squeezing, fullness, or pain.
2. Shortness of Breath
This can occur with or without chest discomfort and involves a sudden difficulty in breathing. It might feel like you’ve just run a marathon, even though you haven’t moved.
3. Other Upper Body Pain
Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw, or stomach. This pain may vary intensely and could feel more like an unusual discomfort rather than sharp pain.
Less Common Symptoms
These symptoms might not be immediately thought of as being related to the heart but are important indicators:
1. Cold Sweat
A sudden cold sweat without physical exertion could be a warning sign of a heart attack.
2. Nausea or Vomiting
Feeling suddenly nauseous or vomiting can be another less common symptom, especially important for women.
3. Lightheadedness
Along with other symptoms, feeling dizzy or lightheaded — especially if also experiencing chest discomfort or shortness of breath — can signal a heart attack.
Atypical Symptoms in Women
Individuals assigned female at birth (AFAB) often experience symptoms that differ from the classic chest pain or discomfort resembling indigestion. Instead, they are more prone to experiencing symptoms such as shortness of breath, fatigue, and insomnia, which may begin before the heart attack occurs. Additionally, they may encounter nausea, vomiting, or pain in the back, shoulders, neck, arms, or abdomen.
What Causes a Heart Attack?
Heart attacks, medically known as myocardial infarctions, predominantly occur due to a blockage in one or more arteries that supply blood to the heart. This blockage usually results from a buildup of plaque, a combination of fat, cholesterol, and other substances. When a plaque ruptures, a blood clot can form, obstructing blood flow and causing a heart attack. In less common cases, heart attacks can also be triggered by a spasm in a coronary artery, trauma, a blood clot from another part of the body, or conditions causing prolonged low blood flow or oxygen levels to the heart.
Risk Factors for a Heart Attack
Various factors increase the likelihood of experiencing a heart attack, including:
- Age and Sex: Risk increases with age, starting at 45 for those assigned male at birth (AMAB) and 50 or post-menopause for those assigned female at birth (AFAB).
- Family History: A history of heart disease in close family members elevates your risk.
- Lifestyle Choices: Smoking, unhealthy diet, inactivity, excessive alcohol consumption, and drug use contribute to heart attack risk.
- Health Conditions: Diabetes, obesity, high blood pressure, high cholesterol, and a history of specific conditions like preeclampsia are risk factors.
Complications of a Heart Attack
Surviving a heart attack can lead to several complications, varying in severity, including:
- Arrhythmias: Abnormal heart rhythms that can be life-threatening.
- Heart Failure: The heart’s diminished ability to pump blood efficiently.
- Valve Problems: Damage causing improper valve function.
- Stroke: Reduced blood flow to the brain.
- Sudden Cardiac Arrest: Unexpected loss of heart function, breathing, and consciousness.
- Depression and Anxiety: Common emotional responses post-heart attack.
- Mechanical complications can also occur, especially without prompt treatment.
Diagnosis and Tests for a Heart Attack
To confirm a heart attack, healthcare providers perform several tests:
- Blood Tests: These look for certain enzymes, like cardiac troponin, that leak into the blood from the damaged heart muscle.
- Electrocardiogram (ECG or EKG): Measures the heart’s electrical activity to identify abnormalities.
- Echocardiogram: Uses ultrasound to visualize the heart’s structure and function.
- Coronary Angiogram: Involves X-rays and a special dye to view blood flow through the heart arteries.
- Heart CT Scan and MRI: Offer detailed images of the heart and its blood vessels, showing blockages or damage.
- Exercise Stress Test: Assesses heart blood flow and performance under physical exertion.
- Nuclear Heart Scans: Use radioactive dye to highlight areas of the heart receiving insufficient blood flow or damaged by a heart attack.
Recognizing the symptoms and understanding the causes and risk factors of heart attacks is crucial for prevention and early intervention, which can significantly improve outcomes. If you suspect you or someone else is having a heart attack, seek emergency medical help immediately.
Heart Attack Prevention
Preventing a heart attack is crucial and largely hinges on lifestyle choices and managing underlying health conditions. Here’s how individuals can lower their risk:
Lead a Heart-Healthy Lifestyle
- Quit Smoking and Avoid Secondhand Smoke: Smoking cessation reduces coronary heart disease risk significantly.
- Eat a Balanced Diet: Favor fruits, vegetables, whole grains, nuts, lean protein, and fish while limiting saturated fats, sodium, and sugar.
- Exercise Regularly: Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week.
- Maintain a Healthy Weight: Being overweight increases heart attack risk, especially around the abdomen.
- Limit Alcohol: Excessive consumption can raise blood pressure and fatty levels in the blood.
Manage Medical Conditions
- Monitor Your Heart Health: Regular check-ups for blood pressure, cholesterol levels, and diabetes management are essential.
- Control High Blood Pressure and Cholesterol: Through diet, exercise, and medication as prescribed by a healthcare provider.
- Manage Stress: Practice stress-reducing activities like meditation, deep breathing, and mindfulness.
Life After a Heart Attack
Surviving a heart attack means confronting the reality of your heart condition and making necessary lifestyle and health adjustments to prevent another episode. Here are key aspects of managing life after a heart attack:
Medical Follow-Up
- Rehabilitation: Cardiac rehabilitation programs provide tailored exercise, education, and counseling.
- Medication Adherence: Continue taking prescribed medications to manage heart disease and prevent complications.
- Monitor Your Health: Regular check-ups with your healthcare provider to adjust treatments as needed.
Lifestyle Modifications
- Dietary Changes: Adopt a heart-healthy diet that supports overall well-being.
- Physical Activity: Gradually return to physical activity, guided by health care providers or through cardiac rehab programs.
- Emotional Health: Seek support for dealing with depression, anxiety, or any emotional distress post-heart attack.
Social and Emotional Support
- Community Support Groups: Joining heart attack survivors’ groups can offer encouragement and understanding of shared experiences.
- Family and Friends: Lean on your support network for help with lifestyle changes and emotional support.
Adjusting to New Normals
- Activity Levels: Understand and respect your body’s new limits and gradually increase your activity levels.
- Sexual Activity: Consult with your healthcare provider about when it’s safe to resume sexual activity.
Life after a heart attack involves significant adjustments, not just for the survivor but also for their loved ones. Embracing these changes can lead to a fulfilling life, reducing the chances of another heart attack.
Vital Heart & Vein: Your Partners in Heart Health and Recovery
Navigating the complexities of heart health can seem daunting, whether you’re looking to prevent heart disease or adapting to life after a heart attack. However, you’re not alone on this journey. At Vital Heart & Vein, we pride ourselves on providing compassionate, state-of-the-art care to all our patients. Home to some of the leading cardiologists in the Houston area, our team is dedicated to supporting you with personalized treatment plans that align with your unique health needs.
Beating Heart Disease is our priority, and we stand ready with the expertise and the latest medical advances to help you live a healthier, fuller life. Whether you are taking preventive steps against heart disease or seeking to regain strength after a heart attack, Vital Heart & Vein is here to guide you every step of the way. Let us be a part of your journey towards better heart health.
